5 surgical procedures where robotic-assisted surgery prevails
Strasbourg, August 4, 2025
In 1985, the first robot-assisted surgical procedure was performed using the PUMA 560 system, which was used to guide a brain biopsy. In the 2000s, the introduction of the da Vinci robotic system marked a decisive turning point, enabling more precise movements, smaller incisions, and 3D visualization, ushering in a new era for robotic surgery.
In 2001, a symbolic milestone was reached in Strasbourg with the Lindbergh Operation, the first telesurgery procedure ever performed. This groundbreaking event confirmed the immense potential of robotic-assisted techniques and firmly positioned Strasbourg as a key player in this surgical revolution.
Twenty-four years later, in July 2025, the city once again hosted a landmark event in the field: the Society of Robotic Surgery (SRS) annual congress, which brought together global leaders in robotic surgery to explore the latest advances and discuss future directions for the discipline.
On this occasion, we take a closer look at 5 types of procedures in which robotic-assisted surgery has become the standard approach, examining the technological innovations, clinical benefits for patients, and the remaining challenges to overcome.

Professor Marescaux remotely controls the ZEUS robot from New York, operating on a patient in Strasbourg during the Lindbergh operation Source: https://www.ircad.fr/fr/linstitut/a-propos-de-lircad/
1. Radical Prostatectomy
Radical prostatectomy is one of the pioneering fields in robotic-assisted surgery. The robot-assisted approach has become predominant, largely due to its demonstrated benefits in surgical precision and functional recovery.
Multiple studies have reported reduced blood loss, shorter hospital stays, and improved preservation of erectile and urinary functions compared to open or laparoscopic surgery (Ho et al., 2011). These advantages have led to widespread adoption, particularly in the United States, where robotic-assisted procedures now account for the majority of radical prostatectomies performed (Ferrari et al., 2024).

CMR Surgical VERSIUS surgical robot
Sources: https://www2.cmrsurgical.com/ | https://www.ircad.fr/fr/new-partnership-with-ircad/
2. Partial or
Total Nephrectomy
Renal surgery, particularly partial nephrectomy, has also greatly benefited from robotic assistance.
A systematic review by Crocerossa et al. (2022) demonstrated that robot-assisted radical nephrectomy is associated with fewer perioperative complications and shorter hospital stays, without compromising oncological outcomes. Regarding partial nephrectomies, Shiroki et al. (2022) highlighted the superiority of the robotic approach over laparoscopy in terms of tumor resection precision, renal function preservation, and complication rates.
3. Colorectal
Surgery
In the colorectal field, robotic surgery is rapidly advancing, particularly for proctectomies and colectomies.
Liao et al. (2022) conducted a meta-analysis including four randomized trials, concluding that robotic procedures result in lower blood loss and reduced conversion rates to open surgery. Another study (Lin et al., 2023) suggests that integrating Enhanced Recovery After Surgery (ERAS) protocols further amplifies the benefits of robotic surgery, with positive effects on hospital stay duration and return of bowel function.
4. Hernia Repair
Robotic surgery has also found its place in hernia repair, especially for inguinal and complex incisional hernias.
A recent review (Peñafiel et al., 2024) showed that compared to laparoscopy, the robotic approach is associated with lower postoperative complication rates and improved cosmetic outcomes. For patients, this often translates into a faster return to daily activities. Iraniha & Peloquin (2018) also reported good long-term quality of life following robot-assisted inguinal hernia repair using the TAPP approach.

Hernia repair using the Da Vinci Si surgical robot from Intuitive Surgical
Source: https://www.intuitive.com/ | https://www.melbourneherniasurgery.com.au/robotic-hernia-repair.html
5. Benign Hysterectomy

Medtronic’s Hugo surgical robot
Source: https://www.medtronic.com/ | https://www.medicaldevice-network.com/news/medtronics-hugo-robot-debuts-at-guys-and-st-thomas-hospital/
Gynecologic surgery has also been profoundly transformed by robotic technology.
A meta-analysis by Lenfant et al. (2023) compared robotic hysterectomy with its laparoscopic, vaginal, and open counterparts. The study found that the robotic approach is associated with lower blood loss, shorter hospital stays, and reduced overall morbidity. However, these clinical benefits must be weighed against the higher associated costs, a factor frequently discussed in the literature.
Conclusion
Robotic surgery does not replace the surgeon, it enhances their capabilities. It enables a level of precision that is often difficult to achieve with conventional laparoscopic techniques. While not all hospitals are yet equipped with robotic systems, the trend is clear: in many surgical specialties, robotics is becoming an essential tool in the operating room, and future advancements will only expand its scope.
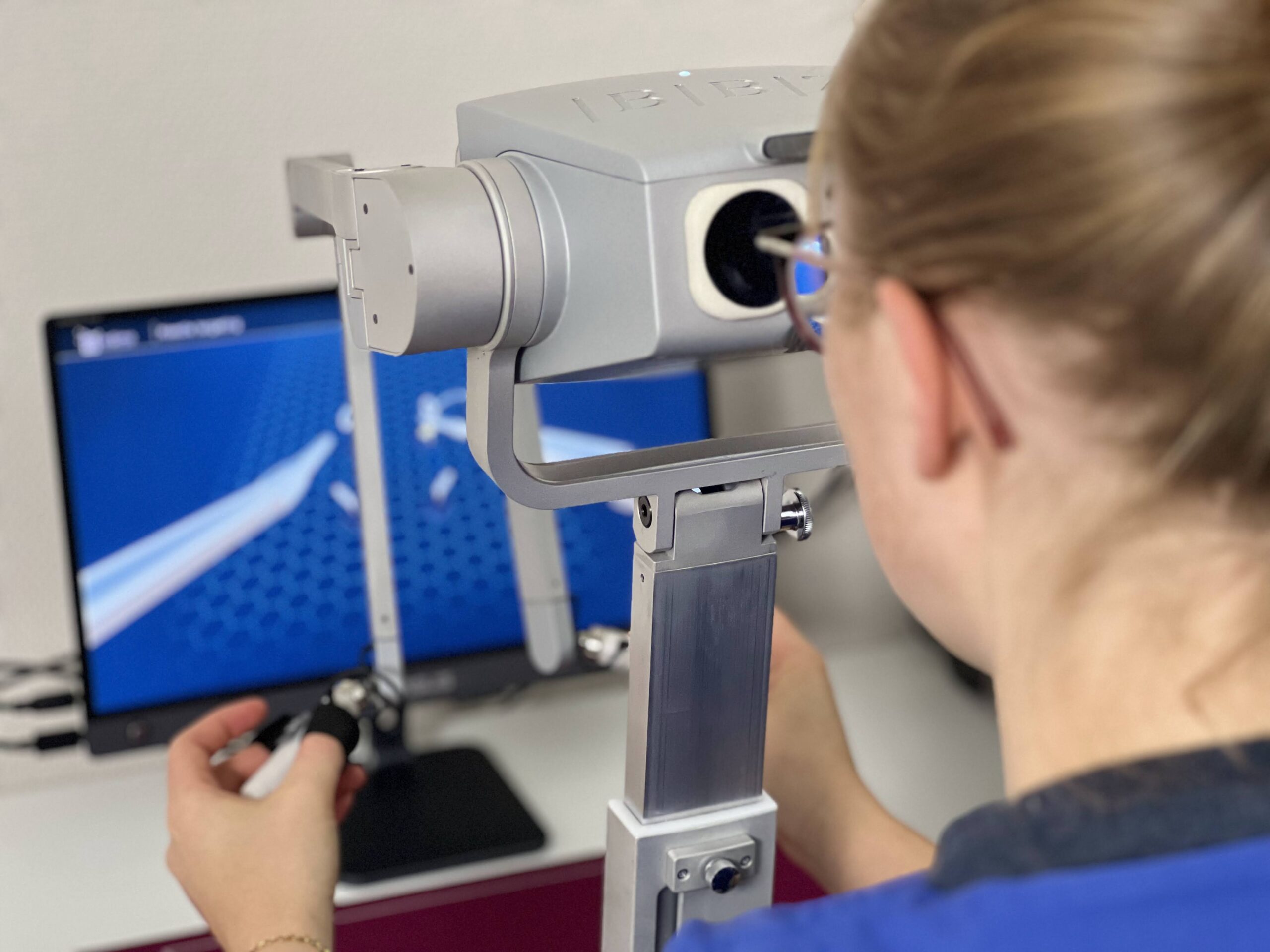
To support the continued rise of robotic surgery, surgeon training is essential. The ROBOTiS simulator offers a highly realistic experience, featuring an unmatched modeling of suture thread dynamics, enabling precise training in robotic maneuvers. Portable and adaptable to all skill levels, it contributes to improved safety in robot-assisted procedures.