How to prepare for a pleural tap?
Strasbourg, September 11, 2025
A pleural tap, also called thoracentesis, is a medical procedure recommended when there is an abnormal build-up of fluid in the pleural cavity. This condition is known as a “pleural effusion”. It can appear suddenly or develop gradually over time, often causing chest pain, a dry cough, and shortness of breath1.
The procedure allows doctors to remove the fluid that has collected between the two thin layers of tissue, called the pleura, which protect the lungs.
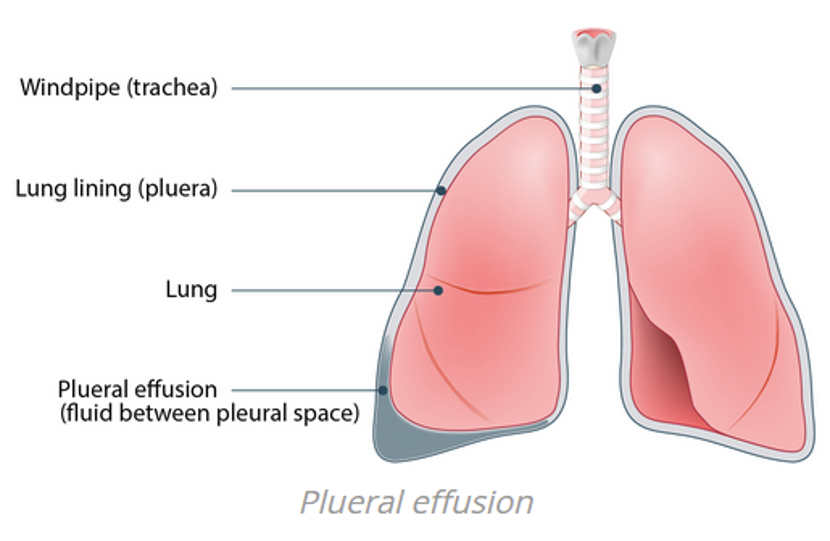
Illustration of a pleural effusion
(Source: Healthdirect)
While thoracentesis is a common procedure, it is still technically delicate and can cause some anxiety for patients who are unsure of what to expect. Understanding its purpose, how it is carried out, and the possible risks can help you feel more at ease and better prepared.
Why is thoracentesis performed?
Thoracentesis is a frequently performed procedure in hospital settings, especially in pulmonology, internal medicine, oncology, and emergency care2.
It has two main purposes:
Diagnostic: to analyze the type of fluid present and determine its cause.
Therapeutic: to relieve breathing difficulties caused by fluid build-up. In this case, the liquid is removed either with a syringe under local anesthesia or, if necessary, through chest drainage3.
How does the procedure work?
To diagnose a pleural effusion, your doctor may use a physical exam along with imaging tests such as a chest X-ray, ultrasound, or CT scan. These help identify the amount of fluid and its exact location4.
Once the diagnosis is made, no special preparation is required:
There is no need to fast
Hospital admission is usually unnecessary
The procedure typically takes about 15 minutes or longer, depending on the amount of fluid5
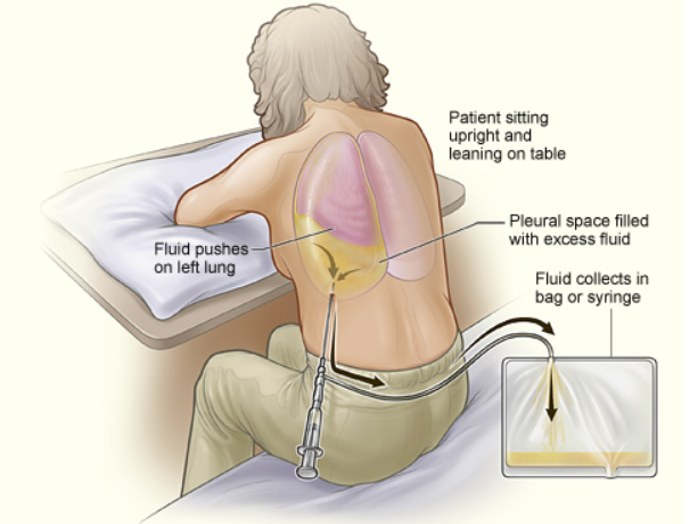
Illustration of the procedure
Source: Institut Mutualiste Montsouris, 2020
The procedure, step by step5:
The patient will sit on the edge of a bed or chair, leaning slightly forward with your arms resting on a table.
After numbing the area with a local anesthetic, the doctor makes a small incision.
A fine needle or trocar is inserted between two ribs in your back to reach the pleural cavity.
The fluid is then withdrawn with a syringe or drained into a bottle.
A small dressing is applied afterward, and in some cases, a follow-up chest X-ray is prescribed.
Risks and possible complications
In most cases, a pleural tap is well tolerated. The use of imaging guidance greatly reduces the likelihood of serious complications. Still, as with any medical procedure, there are some risks to be aware of:
Pneumothorax (collapsed lung): this can happen if air enters the pleural space because the needle touches the lung. Sometimes the air is reabsorbed naturally; in other cases, a chest drain is needed.
Fainting: this can occur due to stress or if the patient has not eaten.
Temporary dry cough: This may appear at the end of the procedure or a few hours later, caused by the lungs re-expanding. It usually doesn’t last long6.
A common but technical procedure
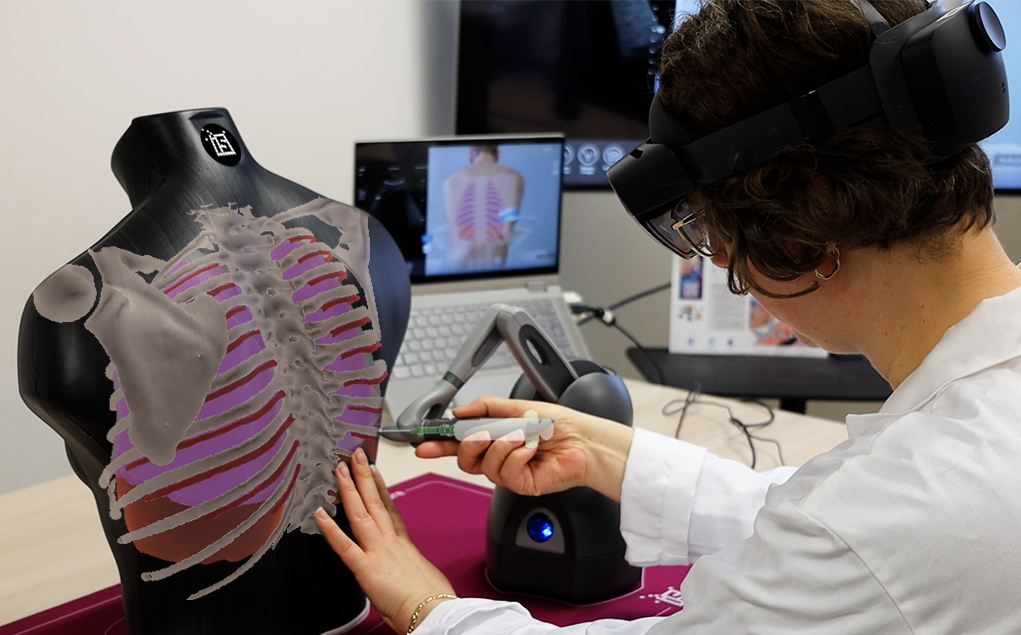
Thoracentesis is a routine but not insignificant procedure. Because it requires precision, many medical schools emphasize the importance of simulation-based training before young doctors perform it on real patients.
Sim&Care | Chest simulator uses augmented reality and realistic force feedback to recreate the experience of performing a pleural tap. This allows students to practice in a safe, risk-free environment that closely mimics real-life conditions, helping them build confidence and skills without causing discomfort to patients.