Complication factors in a lumbar puncture:
how students can prepare with Sim&Care
__
By Héloïse Guillot / 18th August 2021
What are the complication factors during a lumbar puncture?
During a lumbar puncture, the doctor may face different difficulties, such as hitting a bone structure, not correctly identifying the ideal needle path, or touching a nerve in the ponytail. These difficulties increase the risk of procedure failure, and pain or complications for the patient.
Usually, lumbar puncture is performed without anesthesia for the patient, especially in emergency situations. In some cases, the patient may benefit from local anesthesia, but will still be fully conscious. Since lumbar puncture is an invasive and particularly stressful medical procedure, the patient’s state of consciousness can make the gesture complicated for a student who will have to manage both their own anxiety, but also the patient’s stress. In addition, the pain can cause uncontrolled movements in the patient and increase the difficulty.
The success of a lumbar puncture also depends on the morphology of the patient. Age and degenerative or congenital diseases of the spine, as well as obesity, are factors that can influence the outcome of the procedure. These conditions can obstruct the interspinous space, and make it difficult to insert the needle. Scoliosis involving a deformity of the lumbar spine can also distort the trajectory of the needle during the procedure. In patients with a high BMI, locating anatomical landmarks during the palpation step can be complicated, and lead to misidentification of the puncture site. In addition, the doctor must adapt to the morphology of his patient, choosing the right needle gauge according to the distance from the skin to the spinal canal, which is more important in people with obesity.
Possible complications?
Depending on the quality of the procedure, certain complications may appear, including: hematomas or hemorrhages, infections, or even cerebral herniation. The most serious are also the rarest, and are generally avoided by taking the patient’s contraindications seriously into account.
The most common complication is Post Lumbar Puncture Syndrome (PLPS). It manifests as a headache that can last for up to a week after the procedure and can come with nausea and vomiting. It is caused by cerebrospinal fluid (CSF) leaking from the needle breach in the dura and occurs in nearly 40% of patients. Although generally benign, post lumbar puncture syndrome can be particularly invalidating.
The most effective measure to reduce the incidence of PLPS is the use of an atraumatic needle which reduces the incidence to 10%. The bevel of conventional needles causes lacerations in its path, while atraumatic needles separate the fibers without damaging them, thus preventing the leak of CSF. However, they are thinner and more flexible, and therefore require the use of an introducer to pass the skin, which makes the procedure slightly more complex.
How Sim&Care takes these factors into account?
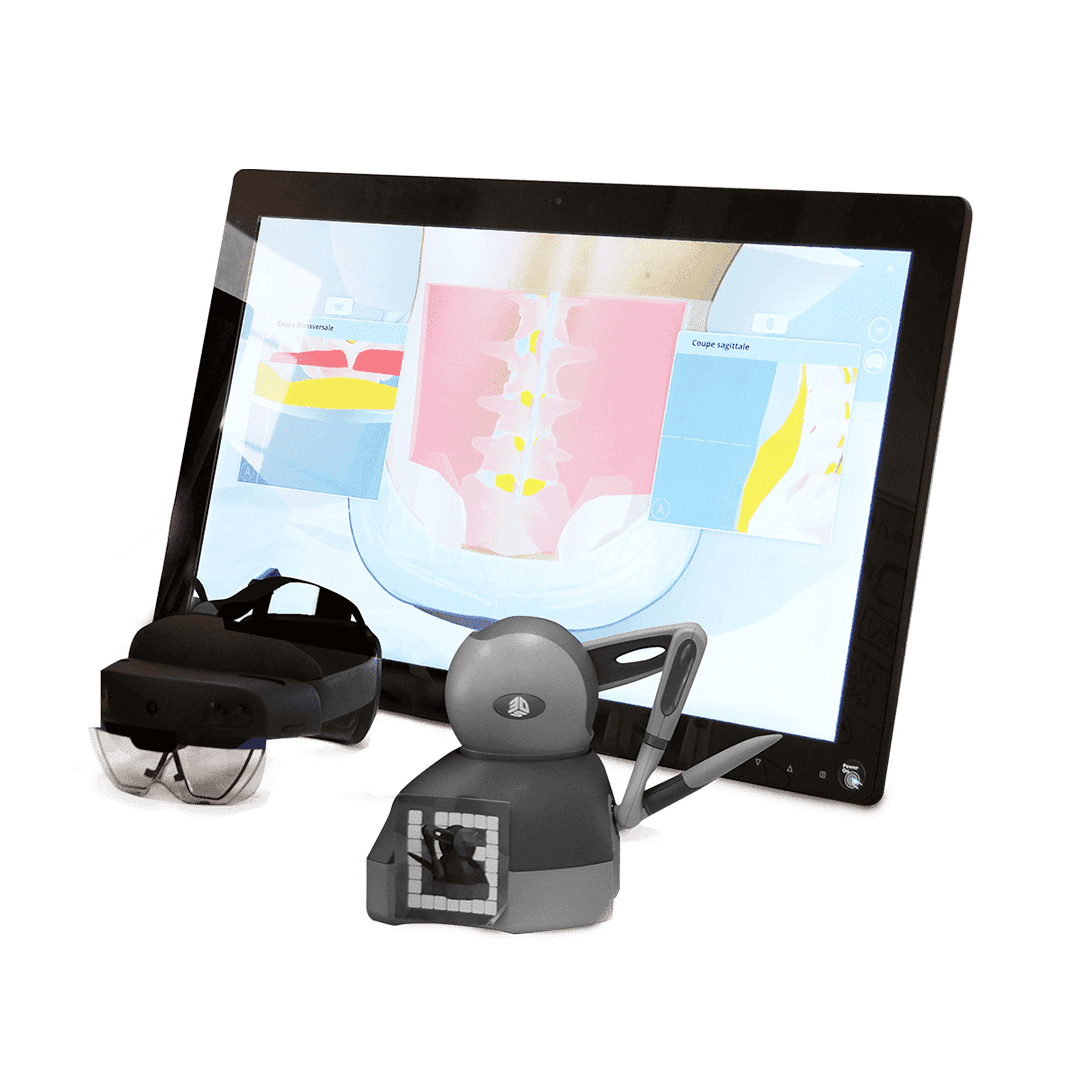
In order to integrate this aspect into our simulator, InSimo has developed a sound immersion synchronized in real time with the simulation. It transcribes the patient’s emotions through sounds, allowing the student to understand the emotional state of his patient. In addition, the patient reacts to the procedure by verbalizing his concerns, and the student can benefit from the instructions of a trainer who helps him acquire the right reflexes.
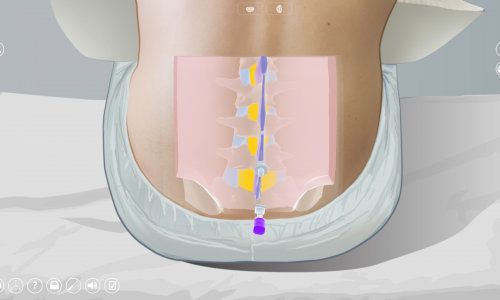
It is also essential that the student be confronted with various morphologies during his practical training. Sim&Care offers a library of different patient cases, which allows students to train on a patient with scoliosis, or on an elderly person, particularly affected by lumbar osteoarthritis. Being confronted with these particular anatomical features prepares the student for the difficulties he may encounter in real patients.

Scoliosis patient in Sim&Care